ACEI or ARB?
Lowering high blood pressure is associated with significant reduction in all major cardiovascular events, all-cause mortality, stroke, coronary events, and heart failure.
Since medicine is still not personalized neither particularly precise, guidelines for choosing the right drug keep evolving. For adults with hypertension requiring pharmacological treatment, the following three classes of pharmacological antihypertensive medications are used as an initial treatment: diuretics, ACE inhibitors or ARBs, and calcium channel blockers.
ACE inhibitors (ACEIs) reduce the activity of the angiotensin-converting enzyme (ACE) which is responsible for hormones that help control blood pressure.
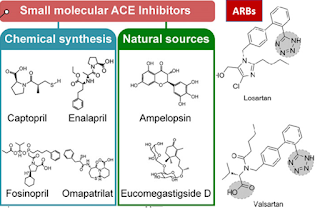
Synthetic ACE inhibitors, such as captopril, enalapril, lisinopril, and temocapril, are in clinical use for the treatment of hypertension. Lisinopril is found to have significant negative effect on perceptual motor skills, thus other ACE inhibitors such as Benazepril, Fosinopril, Moexipril and Perindopril may be better options for certain people. Perindopril is especially beneficial for people with particular genetic variations in angiotensin II receptor type 1: rs5182 and rs275651, and in bradykinin receptor B1: rs12050217. On the other hand, rs1044147 variation in transcription activator polycomb group ring finger 3 is associated with side effects in response to Enalapril while rs1799752 in Angiotensin Converting Enzyme is associated with increased clinical benefit to enalapril or lisinopril (vs benazepril and perindopril) in men with hypertension. Studies not-exploring genetics indicate that perindopril is superior to enalapril in producing monocyte-suppressing and systemic anti-inflammatory effects in normotensive patients with coronary artery disease. n patients with systolic heart failure, perindopril significantly improves cardiac sympathetic nerve activity and brain natriuretic peptide. Additionally, when patients were switched from enalapril to perindopril, left ventricular ejection fraction at 6 months was significantly greater.
However, synthetic ACEI drugs may have certain side effects such as cough, taste disturbances, skin rashes, and drug-drug interactions, which can make them less desirable for some patients. For example, people with the kidney condition bilateral renal artery stenosis (BRAS) should avoid these drugs.
Natural ACE inhibitors, such as those found in plants and functional foods, are being researched as alternative options to synthetic drugs. These natural inhibitors may be considered milder and safer compared with synthetic drugs. Studies have found that phytochemicals and lead compounds derived from plants can also serve as natural ACE inhibitors.
Angiotensin receptor blockers (ARBs) work by blocking the effects of angiotensin II, a hormone that narrows blood vessels and raises blood pressure. ARBs are similar to ACE inhibitors in the treatment of hypertension. ARBs include losartan, valsartan, and candesartan.
Studies suggest that ARBs may be less likely to cause adverse effects, particularly dry cough which is common in ACE inhibitors. ARBs could work better than ACEIs in particular cases. Peripheral Blood Mononuclear Cells (PBMCs) from Rheumatoid Arthritis (RA) patients have been shown to be responsive in inhibiting proinflammatory cytokines using Losartan better than Enalapril and Valsartan and it could be a better antihypertensive choice for patients with RA and systemic arterial hypertension treatment. The ACE inhibitor perindopril was shown to reduce the levels of IL1β in patients with stable coronary disease and in essential hypertension. Losartan was able to reduce levels of IFN-γ (p = 0.0181), IL-6 (p = 0.0056), IL-17F (0.0046) and IL-22 (p = 0.0234) in RA patients. Patients in remission and mild score (DAS28<3.2 and CDAI<10) had a better response to treatment but patients in moderate and severe activity had poor response to Losartan in cytokine inhibition. ARBs were slightly superior to ACE inhibitors for the secondary outcomes of withdrawal due to adverse effects, based on a high level of evidence (RR = 0.83; 95% CI, 0.74 to 0.93; number needed to treat for an additional beneficial outcome = 55 over 4.1 years), mainly because of a higher incidence of dry cough with ACE inhibitors. Dry cough accounted for 43% of the reported adverse effects in the ACE inhibitor arm vs. 4% in the ARB arm. Patients who stopped taking their ACE inhibitor also cited such adverse effects as atrial flutter, edema, rash, and rise in creatinine levels. For those taking ARBs, the reasons for discontinuation of therapy included dizziness, hypotension, palpitations, and dyspnea.

Comments
Post a Comment